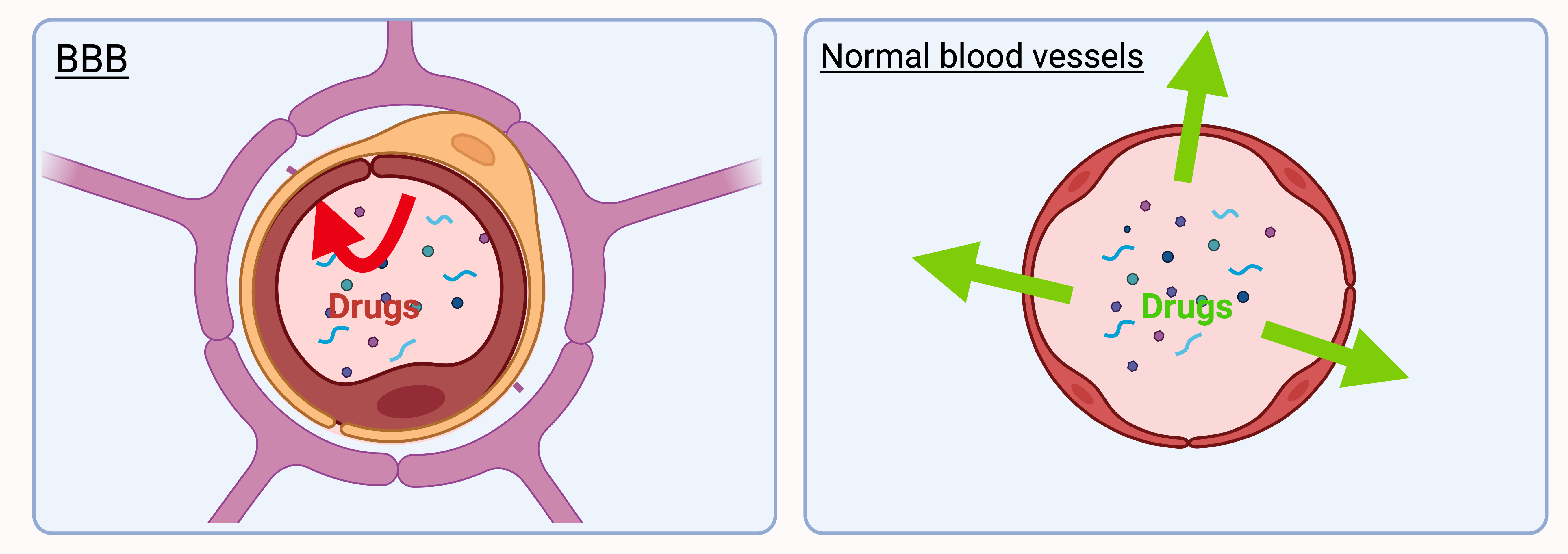
The central nervous system is protected by what is known as the blood-brain barrier (BBB), which prevents toxic molecules from reaching the brain, but also limits the accumulation of drugs in therapeutic doses. The BBB is in fact a barrier around the blood vessels that supply the brain, preventing foreign molecules circulating in the blood from entering the central nervous system.
Of course, some molecules can cross the BBB, particularly if they are small, rather soluble in fats (“lipophilic”) and not highly ionised, but in most cases the development and transfer to patients of molecules with high therapeutic potential are limited by their poor penetration of the BBB.
For this reason, many researchers are working on strategies to improve drug access to the brain.
Some of these strategies may be invasive (direct injection into the brain), but are ill-suited to chronic diseases such as MS. A more acceptable option is to temporarily open the BBB, either with a hypertonic solution or physically, e.g., using focused ultrasound. However, such methods are not very specific, as they open up the BBB to all molecules present in the blood, including potentially toxic molecules.
Alternatively, researchers have developed strategies aimed at using the body’s natural mechanisms to deliver essential substances that are needed by the brain, such as glucose, amino acids, or insulin. These are transferred from the blood to the brain via carriers or specific receptors on the surface of blood vessels in the BBB. It is therefore possible to alter a therapeutic molecule in such a way that the body considers it to be one of these elements and enables it to cross the BBB. This requires that the molecule be chemically modified without altering its therapeutic action, which is not always possible and needs to be optimised for each individual molecule.
Another option is to encapsulate the molecule in a vehicle known as a nanomedicine. These nanomedicines are small spherical particles of nanometric size (generally between 100 and 200 nm) that can carry a whole range of molecules. The surface of these nanomedicines can be modified so that they interact with the receptors or carriers in the blood vessels of the BBB. The advantage is that nanomedicines protect fragile therapeutic molecules, solubilise them if they are not soluble in water, and enable their transport. Also, compared with direct modification of the molecule, a molecule cannot be inactivated by encapsulation in a nanoparticle, and once the nanomedicine or its surface has been modified, it can be used as a vehicle for virtually any molecule.
Finally, another possibility is to change the route of administration. Most drugs are administered either orally or intravenously. However, to avoid the molecule being blocked by the BBB, an alternative route is nasal administration targeting the olfactory mucosa: Nose-to-Brain or N2B. In this case, administration is non-invasive, and the molecule can pass through the olfactory mucosa and reach the brain directly.
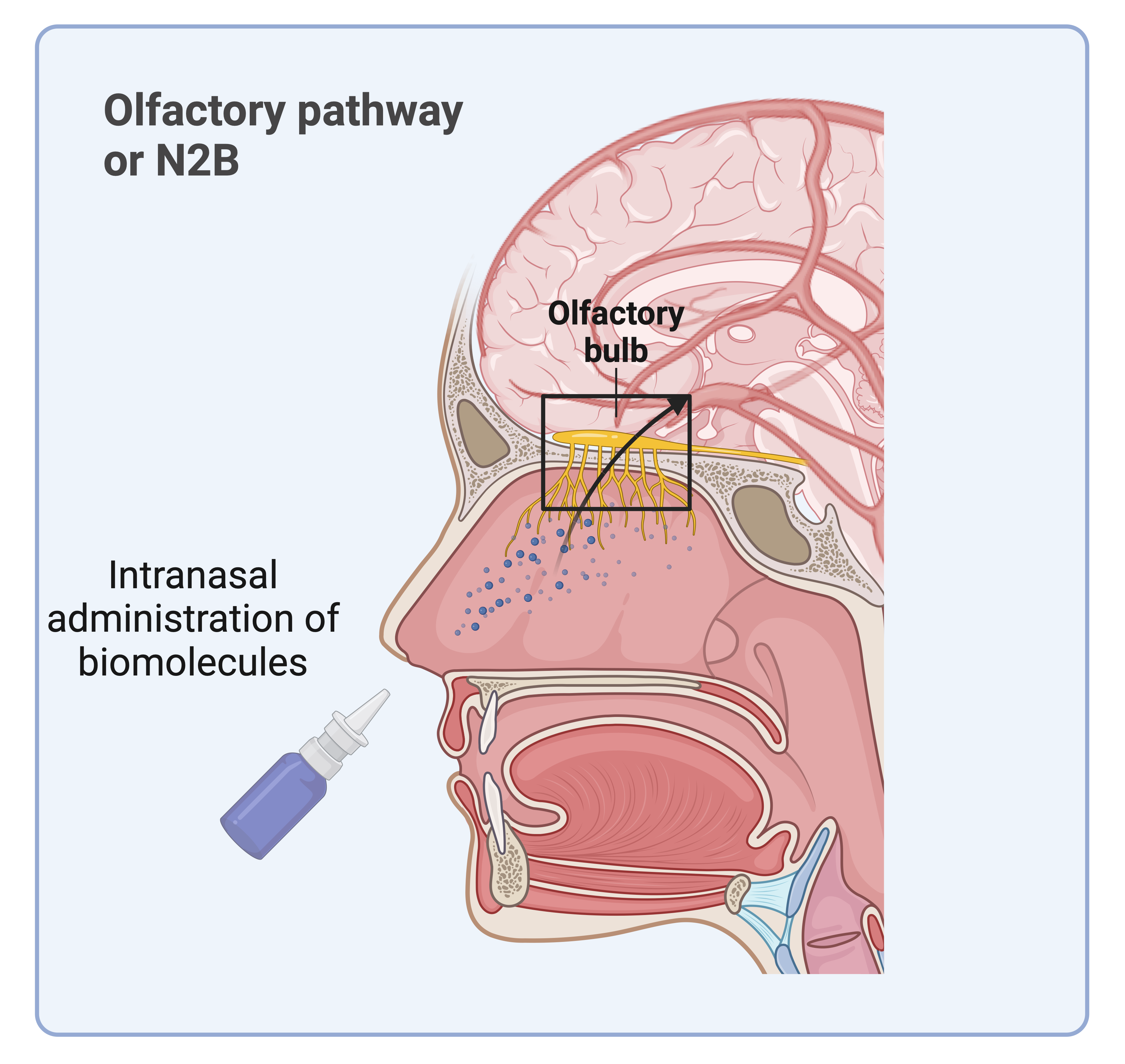
Of course, there are limitations, since a drug passing through the nasal mucosa also enters the bloodstream. But more and more work is aiming to develop this route, either by offering nasal sprays that allow preferential delivery to the olfactory zone (Optinose™), or by adjusting the way in which drugs are formulated, including nanomedicines, so that they pass the olfactory barrier more easily.
Prof. Anne des Rieux, Louvain Drug Research Institute, UCLouvain
